In 2021, Carilion Clinic, a $2 billion revenue, eight-hospital integrated system in Roanoke, Virginia, was facing a problem familiar to many systems around the country: stubbornly high average length of stay (ALOS) hurting Carilion’s efforts to serve its community.
The pandemic had exacerbated operational challenges and mitigated the effectiveness of previous interventions, driving key metrics in the wrong direction. Not only was inpatient ALOS a challenge, but Carilion also identified rising observation rates, suggesting an opportunity to improve how it classified patient status.
To tackle both issues at once, Carilion partnered with members of then-Claro Healthcare, which is now part of Kaufman Hall, a Vizient company. Their joint implementation efforts—encompassing people, process, and technology, with associated monitoring and oversight—produced results well-beyond initial projections.
Kaufman Hall and Carilion’s partnership
"When a healthcare system collaborates with a consulting firm, it necessitates that system leaders adapt, adopt, and integrate external expertise into their teams. Given the inherent complexity of healthcare systems, sophisticated approaches are essential, particularly when aiming to become a high-reliability organization. Leaders who lack professional experience with consulting projects might hesitate to engage, fearing that the project reflects on their abilities or that external help is unnecessary. They may not fully grasp that the challenges faced by intricate health systems surpass individual capabilities. These engagements temporarily augment resources for teams without necessitating permanent staff increases and further educate leaders to improvement strategies.
Executives might also bring in consulting partners due to existing pressures on the leadership team, while recognizing the need for additional improvements. The demand for change management, along with increased resources, is substantial in health systems. Leaders might believe that continuing past practices will ensure future success, but consulting firms can facilitate change, focus resources on critical areas, and introduce external best practices to enhance access and quality of care."
—Paul Davenport, System Senior Vice President, Carilion Clinic
Project parameters and approach
Kaufman Hall (formerly Claro Healthcare)’s engagement with Carilion began in March 2021 with an assessment of the challenges before them. Over the previous 2.5 years, inpatient ALOS and observation rates had increased. These troubling trends were reframed as opportunities for improvement that could reap significant benefits to Carilion, both financially and for their mission, if abated or reversed.
Implementation was a multi-layered process covering the planning, designing, and integrating of improvement initiatives. To turn these theoretical improvements into reality, Kaufman Hall and Carilion worked together to engage with and educate the staff, creating organizational awareness and buy-in. The team enhanced the current multidisciplinary forums and implemented additional workflow improvements. They also stood up dashboards that tracked key metrics, incorporating these tools into their educational efforts.
The monitoring and support phase involved monthly reporting on financial and operational progress, chart reviews, and on-site visits for educational follow-up. Beginning with implementation, the executive steering committee met each month to exercise overall project responsibility, but its work during the monitoring phase shifted toward ensuring sustainability for the project by empowering the front-line staff and director-level process owners. While members of the Kaufman Hall team led the initial steering committee meetings, leaders at Carilion took increasing charge of the meetings over the course of the engagement.
Results, challenges, and keys to success
From FY2021 to FY2024, Carilion Roanoke Memorial Hospital (CRMH) saw its inpatient ALOS drop by 0.5 days, which translated to more than 8,000 additional inpatient admissions in that time period relative to pre-intervention trends (Figure 1). Its observation ALOS was reduced by more than five hours and its observation rate was lowered by 4.5 percentage points from the first to final year as well (Figure 2). All of these figures met or exceeded initial projections established during the assessment phase.
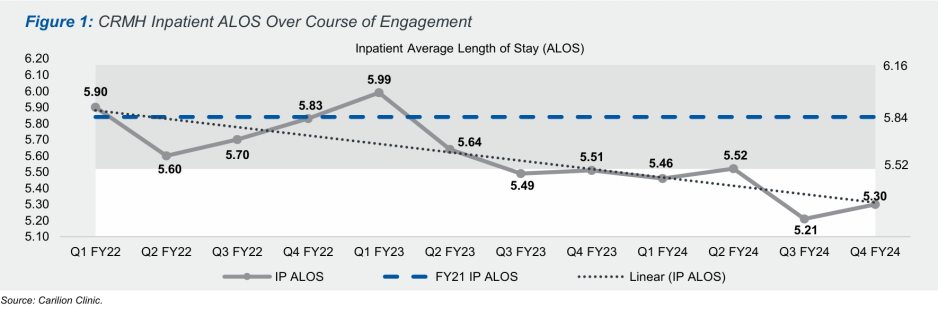
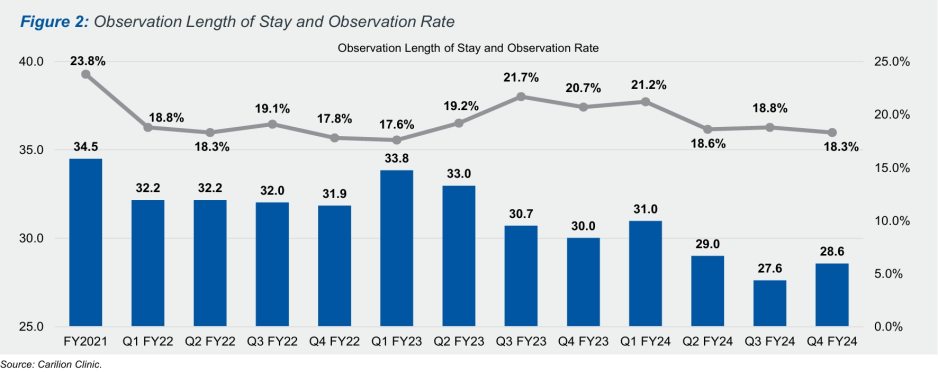
Progress was not always linear, and the team overcame a variety of barriers to achieve these results. Like other health systems during the pandemic, Carilion experienced staffing challenges during the initial rollout which slowed the progress of ALOS reductions in particular. CRMH also experienced bed closures during the engagement, increasing the importance of throughput improvements. In addition to these operational pressures, Carilion underwent key leadership changes during the engagement, which threatened its momentum.
However, these challenges were by and large overcome. The ultimate success of this project can be attributed to a number of factors, such as the following:
- Effective multi-disciplinary teams
- Bought-in physician leadership
- Skilled case management leadership
- Strong nursing and ancillary accountability
- Trusting relationship between the client and consultants
- Dedicated commitment to change management
- Educated, hand-in-hand support with regular meetings to build consensus
Conclusion and Carilion’s path forward
This engagement owes its success to the hard work and adaptability of Carilion’s leaders and team members, who carried an attitude of “how can we get this done?” rather than a “no we can’t” mentality. Systemwide communication and awareness was a focus throughout the process, and the leadership growth of physicians and other front-line team members laid the foundation for the sustainability of these improvements.
Pairing throughput improvements with patient status determination redesigns also paid off: more immediate progress on the latter helped generate buy-in for the former, amid external operational pressures. The emphasis on having a plan for each patient the moment they enter CRMH’s doors was critical to ensuring the proper patient status and advancing the patient toward a timely discharge.
Today, Carilion’s focus remains set on sustained and continued improvement. Process changes and awareness efforts risk decay as organizational priorities shift elsewhere. Rather than resting on its laurels, Carilion is taking this new standard of care enterprise-wide by applying it to their community facilities as well. Streamlining and standardizing these process changes, continuing to actively monitor and report out results, and setting new, more ambitious goals across the organization will help Carilion stay on a growth trajectory.
Acknowledgements: The authors would like to thank Morgan DeHaan, Anita Tinsley, and Bart Richards for their insights, reviews, comments, and research on this topic.