Greetings, and thanks for your continued readership of the Gist Weekly—as always, please feel free to forward this edition to friends and colleagues, and encourage them to subscribe as well.
In the News
What happened in healthcare recently—and what we think about it.
- Novant cancels plan to acquire two CHS hospitals amid FTC challenge. Winston-Salem, NC-based Novant Health, an $8B, 15-hospital system, called off its plan to purchase two hospitals in the Greater Lake Norman area of North Carolina from for-profit hospital chain Community Health Systems (CHS) on Tuesday, after an appellate court granted the Federal Trade Commission (FTC) more time to challenge the deal. The FTC sued to block the deal in January, claiming the acquisition would harm competition and increase healthcare prices in the region by allowing Novant to control more than 65 percent of the region’s inpatient market share. In two back-to-back rulings earlier this month, US District Court Judge Kenneth Bell denied the agency’s requests to stop the $320M deal, along with its request for a preliminary injunction, pointing to the hospitals’ likelihood of shuttering absent a buyer. The deal seemed near closure until the FTC won on appeal a temporary injunction blocking the sale. Rather than continuing to argue its case, Novant elected to abandon the purchase, with a Novant spokesperson citing the FTC’s “continued roadblocks” to the transaction. CHS then released a statement saying it’s “evaluating the current operations” at the two involved hospitals, but that no immediate changes to healthcare services should be expected in the interim.
- The Gist: The FTC has had mixed results in its recent attempts to block healthcare transactions in court on antitrust grounds. This closely watched case is, at most, only a partial victory for the agency, as it just delayed the deal until Novant abandoned it, rather than achieving an actual legal win. Amid this current era of FTC uncertainty, hospital and health system M&A activity continues to tick up after a pandemic-era slowdown, and the future of Lake Norman Regional Medical Center and Davis Regional Medical Center—the two hospitals at the center of this deal—remains in limbo.
- Amazon expands generic drug subscription service RxPass to Medicare. On Tuesday, Amazon announced that RxPass, its subscription program for generic drugs, is now available to more than 50M Medicare beneficiaries. Launched last year to attract more Prime members to Amazon Pharmacy, RxPass offers Prime members in 46 states (currently excluding California, Washington, Texas, and Minnesota) unlimited prescriptions and free delivery of about 60 common, generic medications for an additional $5 monthly flat fee. Although RxPass does not take insurance, Amazon had to meet additional regulatory and compliance measures required for Medicare beneficiaries to subscribe. (Medicaid recipients remain ineligible) Potential savings for Medicare beneficiaries will depend on their prescription drug plan and which medications they take, but Amazon estimated that a beneficiary who takes at least one medication on its list could save about $70 per year, and if all beneficiaries were to transition their eligible medications to RxPass, Medicare spending could be reduced by nearly $2B per year.
- The Gist: As only “tens of thousands” of Amazon’s nearly 168M US-based Prime members are currently subscribed to RxPass, the program certainly has room to grow. The e-commerce giant’s expansion into the Medicare market should be mutually beneficial, as one in five seniors report medication nonadherence due to costs, and RxPass’ flat-fee pricing model is most attractive for people on multiple medications, as many seniors are. However, Amazon faces significant competition in the direct-to-consumer pharmacy space, including from fellow retailers like Walmart and Costco, as well as from startups like the Mark Cuban Cost Plus Drugs Company.
- DOJ accuses executives at telehealth startup Done of an Adderall distribution scheme. Last Thursday, the Department of Justice (DOJ) announced it had arrested both the CEO and clinical president of Done, a San Francisco-based telehealth company focused on prescribing ADHD medications, in connection to an alleged scheme to “provide easy access to Adderall and other stimulants for no legitimate medical purpose.” Enabled by loosened restrictions on telehealth prescriptions for controlled substances during the pandemic, the DOJ alleges that Done obtained more than $100M of potentially fraudulent revenue by engaging in false-advertising practices and pressuring providers to prescribe stimulants to unqualified patients. In a statement released Tuesday, Done says it “disagrees” with the criminal charges and continues normal operations despite the proceedings. This marks the first time the DOJ has levied charges against a digital health company for its drug distribution practices. Following the indictment, the Centers for Disease Control and Prevention issued a warning that up to 50K patients who have relied on subscription-based telehealth platforms like Done for their ADHD medication, which are already in shortage, may experience disrupted access to care.
- The Gist: Prescriptions for ADHD medications boomed during the pandemic, largely due to relaxed telehealth prescribing regulations for controlled substances. Done may be the first telehealth company to face federal charges for its allegedly fraudulent prescribing behavior, but the DOJ has also investigated mental health telemedicine company Cerebral for “possible violations” of the Controlled Substances Act. The Drug Enforcement Administration (DEA) is close to releasing a final rule for telehealth and controlled substances, as the current flexibilities are due to expire at the end of the year. The DEA proposed two, related rules in March 2023 that would require drugs like Adderall to be prescribed only after an in-person examination.
Plus—what we’ve been reading.
- Chief wellness officers gaining prominence in health systems. Published in Health Affairs last month, this piece highlights how employee wellness has emerged in recent years as a critical challenge for healthcare delivery organizations, given the fact that burnout in the provider workforce remains persistently high. The author, the chief wellness officer (CWO) at the Icahn School of Medicine at Mount Sinai, discusses what he sees as the job description and core job functions of a CWO that enable that leader to help their organization achieve its strategic priorities while supporting its workforce. The author also, importantly, lays out the human resource responsibilities that he believes the role shouldn’t include. He summarizes the mandate of a CWO as helping “the workforce to efficiently and effectively complete its work while feeling part of a culture that values its voice.”
- The Gist: This article emphasizes the strategic importance of improving the wellness of a healthcare workforce that’s still suffering from a deep crisis of morale. Appointing a CWO is one way to demonstrate a commitment to employee wellbeing, but the duties of a CWO are more important than the role itself. Systems hesitant to add another chief to their C-suites should at least ensure that these responsibilities are meaningfully delegated across a handful of other system leaders and tied to measures of accountability. Although a CWO can spearhead employee wellness efforts, the well-being of the workforce remains the responsibility of all leaders throughout the organization.
Graphic of the Week
A key insight illustrated in infographic form.
Highlighting LGBTQ+ healthcare disparities
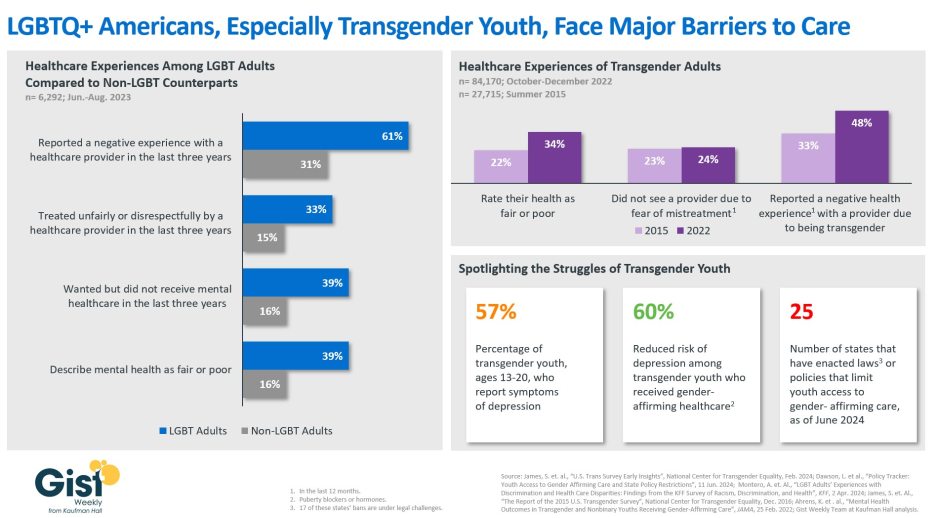
In honor of Pride Month, the graphic below highlights the inequities many members of the LGBTQ+ community report facing when accessing healthcare services. LGBT adults were more than twice as likely to report being treated unfairly by a healthcare provider. Negative experiences or fear of mistreatment can lead to healthcare deferrals that may exacerbate both patients’ physical and mental health, the latter of which LGBT adults are more likely to rate as being poor. Fear of discrimination is particularly pronounced for the transgender community. Nearly half of transgender adults reported a negative experience with a healthcare provider related to their gender identity, and, alarmingly, a larger share reported negative healthcare experiences in 2022 compared to 2015. Within the transgender community, transgender youth face some of the greatest barriers to care, in part due to the proliferation of state policies that limit their access to gender-affirming care. Despite evidence that receiving this kind of care reduces the risk of depression among transgender youth by 60 percent, half of all states have enacted laws to limit access to these treatments, although many of these laws are currently facing legal challenges. The health disparities that persist among the LGBTQ+ patient population must continue to be both acknowledged and addressed as part of the healthcare industry’s greater commitment to health equity.
On the Road
What we learned from our work in the real world. This week from Lance Robinson, Managing Director, at Kaufman Hall.
Addressing organizational culture within performance improvement
A veteran health system CEO I’ve worked with over the years recently called me up to talk big picture about his system, which had a rough go through the pandemic years. “It feels like we’re stuck on first base, still,” he admitted regarding his system’s performance improvement strategy. “We’ve cut back our agency labor, and our inpatient volumes are ticking back up, but our operating margin is still hovering near zero percent. Most of the levers still available for us to pull aren’t going to be popular with our physicians or staff, and our burnout rates are still high. How do we get them on board?”
Tenured health system leaders surely know the go-to playbook for margin improvement. My role in these conversations is usually to get them to look harder at the areas where they usually want to avoid looking—at things like clinical staffing levels, physician preference items, service line rationalization, and payer network strategy—and create a plan that accounts for overcoming the very real cultural barriers to changes in these areas. A structured project management approach that objectively quantifies improvement opportunities with outside benchmarks, sets clear targets tied to both the budget and the strategic plan, and establishes formal accountability measures is needed in any performance improvement undertaking. But the real make or break of performance improvement comes from identifying and elevating internal champions to lead the execution of the various, agreed-upon steps. The structures and frameworks created should serve as tools to convince an organization’s leaders of the necessity for these changes; they in turn can then drive cultural acceptance and accountability downstream. If your organization is grappling with identifying what will really turn the dial in your performance improvement strategy, or struggling to garner better support for the areas of improvement you’re trying to pursue, please don’t hesitate to reach out.
On Our Podcast
Gist Healthcare Daily—all the headlines in healthcare policy, business, and more, in ten minutes or less every weekday morning.
Although the podcast was dark this week, Stephanie Wolf—in for J. Carlisle Larsen—will be back on Monday with regular news episodes. We hope you tune in daily to keep abreast of the latest news.
Subscribe on Apple, Spotify, Google, or wherever fine podcasts are available.
We look forward to you joining us again here next week! Until then, please check out our archive if you’d like to peruse past editions of the Gist Weekly.
Best regards,
The Gist Weekly team at Kaufman Hall






