
Housing affordability—a problem that used to affect primarily the healthcare workforce in large urban centers and high-priced enclaves—is becoming an issue in a growing number of markets. From April 2021 to April 2022, the National Association of Realtors’ Housing Affordability Index dropped from 154.4 to 109.2. This means that the Affordability Index is approaching the threshold of 100, below which a household earning the national median income ($89,985 in April 2022) no longer qualifies for a 30-year fixed mortgage to purchase a median-priced home (estimated at $397,600 in April 2022).
The growing affordability crisis is the product of several factors:
- Remote Workforce: The shift to a more remote professional workforce during the pandemic enabled individuals to move to certain sought-after locations or lower-priced markets, with increased demand driving up housing prices.
- Mortgage Rates: According to data from Freddie Mac, the average rate for a 30-year fixed rate mortgage has nearly doubled over the past year, from around 3% in June 2021 to almost 6% in June 2022.
- Housing Prices: Although inflationary pressures and staffing shortages have led to wage gains, the pace of housing price increases has far exceeded those gains (Figure 1).
- Rental Markets: Pressure on rental markets is increasing as fewer would-be home purchasers can afford to buy a home. The national median asking rent rose above $2,000 for the first time in May 2022, a 15% year-over-year increase.
Figure 1: Home Sale Prices Relative to Income
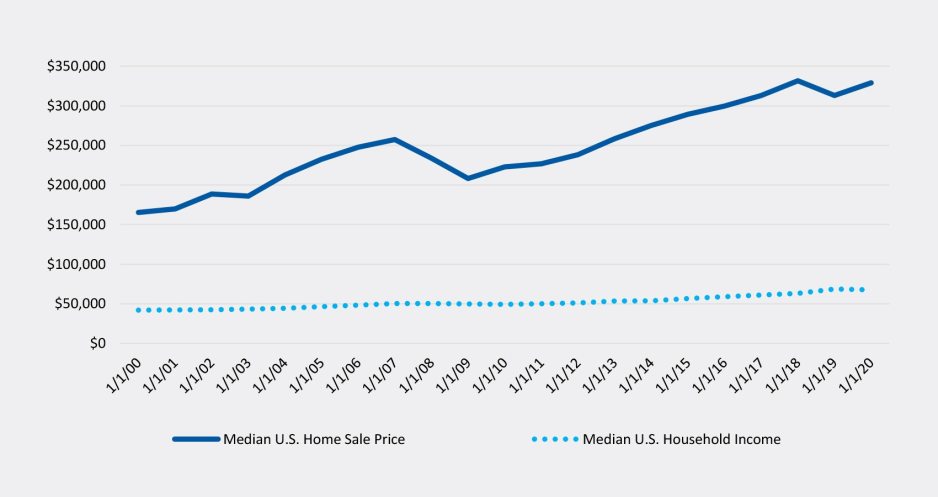
Sources: Zillow, Wall Street Journal, St. Louis Fed, Morning Consult
Impact on health systems
Housing affordability is a significant issue for health systems and has contributed to difficulties with employee recruitment and retention. To help mitigate this issue, health systems may need to raise employee salaries, which would put additional stress on the organization’s cost structure. In some cases, where a substantial portion of the workforce cannot afford to live near the main facilities, the organization may need to pay for or subsidize transportation costs. In a worst-case scenario—for example, a natural disaster requiring a rapid and widespread emergency response—the health system may not have enough employees available locally to adequately respond.
In some markets, the affordability crisis may subside if housing supply is able to catch up with demand, or demand subsides. The housing construction industry has struggled with supply shortages and high material costs during the pandemic. But in many markets, high housing costs are likely to persist. Whether the issue is short term or long term, health system leaders have a variety of options available to address housing affordability for their workforce.
Strategies to address housing affordability
The strategies available to health systems seeking to address housing affordability issues for their workforce include the following:
Conversion of an owned asset. For health systems with certain unused or underutilized facilities, such as administrative buildings, conversion of these assets into housing units may provide housing close to the hospital, while simultaneously improving the overall campus and maintaining future control. Two factors—the dramatic increase in multifamily unit rental rates and a significant amount of office space that is now vacant due to the shift to remote work—have increased interest in this strategy, with a record number of non-residential buildings converted into apartments in 2021.
For-profit partnership. This strategy focuses on partnering with for-profit entities that can assist with financing or the development of housing projects for health systems. Deals can be structured to provide certain benefits to the health system, such as having units designated for health system employee purchase (with potential restrictions on subsequent sales of the units), or preferential treatment when employees are being evaluated as tenants. The for-profit partner can bring tangible real-estate capabilities that ensure successful completion of a project and allow the health system to take a more passive role in the process.
Master or partial lease of an existing housing development. Under this strategy, health systems lease existing homes or apartment buildings and then sublease the units to employees. Health systems can control affordability by adjusting the rent charged for the subleases (which therefore will often be less than the rent paid for the master or partial lease). This strategy provides health systems a quick option to address housing affordability for employees with the flexibility to end a lease if housing in the respective market becomes more accessible.
Alignment with a public entity. Health systems may be able to partner with local, state, or other government entities that similarly are focused on addressing the community’s affordable housing needs. Depending on the partnership structure, the public entity may be able leverage certain resources, such as low-income tax credits, that can reduce the financial burden of a prospective project for the health system. Health systems pursuing this option should anticipate potentially longer lead times and the need for ongoing cross-organizational collaboration.
Not-for-profit partnership. This strategy focuses on partnering with not-for-profit organizations that have a specific mission to develop and maintain affordable housing. Community land trusts (CLTs), for example, are not-for-profit organizations that develop and retain long-term ownership of properties, with permanent rent control established through deed restrictions. A health system might donate vacant land or other property to a partner CLT, which in turn develops affordable housing units and offers preferential treatment to the health system’s employees.
Although many strategies are available, the best option for each respective health system will depend on several factors, including the degree of employee demand for housing, anticipated short- and long-term market conditions, and the health system’s desired level of involvement in the process. Considerations regarding these factors are outlined in Figure 2.
Figure 2: Considerations in Determining Which Strategy to Pursue

Health system leaders should consider any tax implications of providing affordable housing to their employees when assessing available strategies. They should also be sensitive to housing affordability issues for the community as a whole and have a clear communication plan describing the need to focus on their employee population to ensure the community’s health and safety.
Conclusion
We all hope that the housing affordability crisis is a short-term byproduct of social and economic responses to the pandemic and its impacts, but the effects of the crisis on many members of the healthcare workforce—and the health systems that employ them—are very real. Health systems need to understand the scale and potential duration of the issue in their respective markets and scale their responses appropriately. They should also recognize that housing development typically is not part of a health system’s core strategy and that there are potential partners and capital sources that can help them achieve a desirable solution.









